By Barbara Adams and Jens Martens, Global Policy Forum
The COVID-19 crisis continues to have devastating consequences across all sectors, demonstrating the impact of what the 2030 Agenda for Sustainable Development called the "enormous disparities of opportunity, wealth and power" that confront progress on sustainable development goals.[1]
Development economist Jayati Ghosh summarizes the situation as follows:
The perfect storm of COVID-19 and climate change delivers the glaring message that the apocalypse is now. The novel coronavirus mutates into more transmissible, drug-resistant variants, while climate catastrophe plays out in real time.[2]
WHO Director-General Tedros Adhanom Ghebreyesus sounded the alarm in January 2021 not only of a health catastrophe but also of a moral failure:
I need to be blunt: the world is on the brink of a catastrophic moral failure – and the price of this failure will be paid with lives and livelihoods in the world’s poorest countries. Even as they speak the language of equitable access, some countries and companies continue to prioritize bilateral deals, going around COVAX, driving up prices and attempting to jump to the front of the queue. This is wrong.[3]
By May 2021, he was more explicit in his criticism, saying it is “not just that the world is at risk of vaccine apartheid; the world is in vaccine apartheid.… The basic problem is a lack of sharing, so the solution is more sharing."[4]
Global vaccination inequalities
A key challenge in responding to the COVID-19 pandemic is the production and fair distribution of vaccines in order to immunize the entire global population against the virus. This has been the focus of a movement for a Peoples Vaccine that is continuing to gain strength (see Box 3.1).
In adopting the 2030 Agenda and the 17 Sustainable Development Goals, governments worldwide committed under SDG 3 on health and well-being to "Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all". They also committed to:
Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries, provide access to affordable essential medicines and vaccines, in accordance with the Doha Declaration on the TRIPS Agreement and Public Health, which affirms the right of developing countries to use to the full the provisions in the Agreement on Trade-Related Aspects of Intellectual Property Rights regarding flexibilities to protect public health, and, in particular, provide access to medicines for all” (SDG 3b.)
The world is far from achieving this target in the production and distribution of COVID-19 vaccines. By 1 September 2021, about 5.4 billion doses of a COVID-19 vaccine have been administered globally. But while more than 50 percent of people in high-income countries had received at least one dose, the share in low-income countries was only 1.8 percent (see Figure 1.1). In many African countries, the share of people fully vaccinated against COVID-19 was lower than 1 percent.
Figure 1.1: COVID-19 vaccine doses administered by country income group
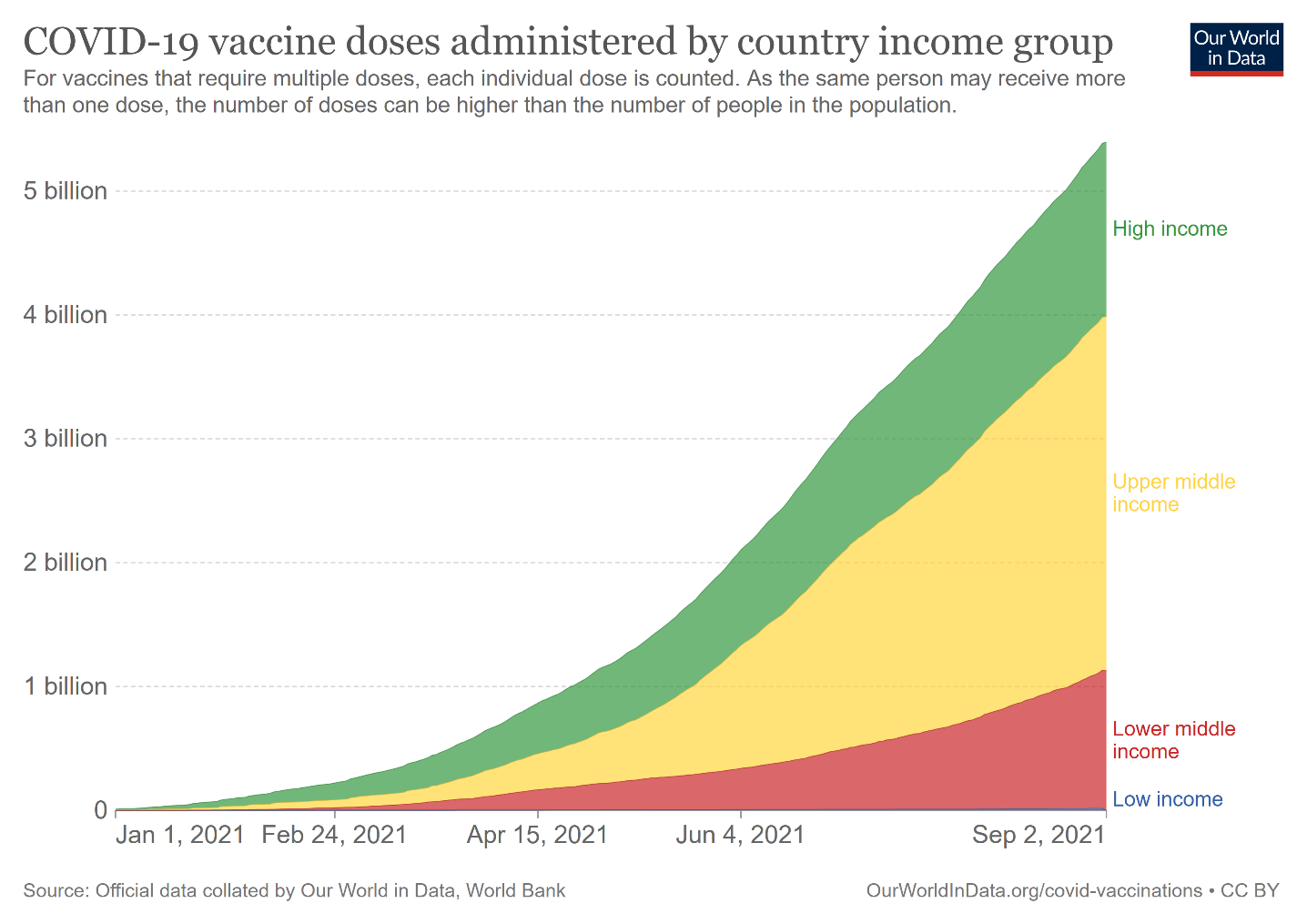
Source: Official data collated by Our World in Data, World Bank (https://ourworldindata.org/covid-vaccinations)
The World Health Organization (WHO) made an early appeal to countries to agree on a coordinated distribution of vaccines, with available doses distributed fairly according to the size of each country's population. This has not happened. The European Commission, the United States, the United Kingdom, and numerous other countries have signed bilateral COVID-19 Vaccine Agreements with vaccine producers to secure vaccine quotas. By the end of August 2021, more than 400 agreements were concluded by these countries,[5] securing over 18 billion doses of vaccine.
The European Commission has so far negotiated supply agreements for 4.1 billion doses of vaccine, equivalent to 8 vaccine doses per capita of the EU population. The UK could vaccinate its population 9 times with the contracted doses, the USA 10 times and Canada as many as 16 times.[6]
Figure 1.2: COVID-19 vaccine supply agreements by the top 10 recipient countries/groups
(number of doses)
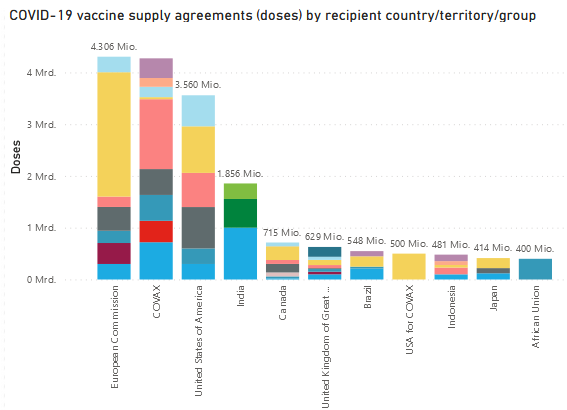
Source: https://www.unicef.org/supply/covid-19-vaccine-market-dashboard (1 September 2021)
Exacerbating the problem for many countries in the global South is the enormous cost of vaccines. Even though supply contracts are secret, more and more price information has been disclosed in recent months. UNICEF publishes it regularly on its Vaccine Market Dashboard (https://www.unicef.org/supply/covid-19-vaccine-market-dashboard). The cheapest dose of the COVID-19 vaccine costs US$ 2.19 (AstraZeneca), the most expensive US$ 37.00 (Moderna). The producers do not charge standard prices, but vary their prices depending on the quantity purchased and the bargaining power of the purchaser.
Occasionally, producers grant preferential terms to rich countries, while countries in the global South sometimes have to pay higher prices. For example, the European Commission received a batch of AstraZeneca vaccine for US$ 2.19, while Argentina had to pay US$ 4.00 and the Philippines US$ 5.00. Pfizer/BioNTech and Moderna's mRNA vaccines are much more expensive. The African Union had to pay US$ 6.75 for one dose of the Pfizer/BioNTech vaccine, while the European Commission had to pay as much as US$ 23.15. Botswana had to pay US$ 14.44 million for 500,000 doses of Moderna vaccine, or US$ 28.88 per dose, while the USA got Moderna's vaccine at almost half the price (US$ 15.00).
The prices of other vaccine manufacturers have similar differences. The price per dose of Chinese manufacturers Sinopharm and Sinovac range between US$ 10 and US$ 36, the Russian Sputnik V vaccine costs between US$ 10.00 and US$ 27.00 per dose. Only the prices of the Serum Institute of India are far below that, at US$ 3.00 to US$ 5.00.
Box 1.1
Skyrocking profits of vaccine producers
The oligopoly of vaccine producers makes exorbitant profits, as the actual production costs of COVID-19 vaccines are many times lower than their market price. According to estimates in a study published by Public Citizen, production costs for mRNA vaccines range from US$ 1.18 (Pfizer/BioNTech) to US$ 2.88 (Moderna).[7]
The U.S. pharmaceutical company Pfizer
expects a massive increase in sales of more than 85 percent from US$ 41.9 billion to US$ 78-80 billion in 2021.[8] Of this, US$ 33.5 billion is attributable to the COVID-19 vaccine alone. Pfizer's net income in the first six months of 2021 increased by 53 percent compared to the same period in 2020, to US$ 10.4 billion.[9]
Pfizer's German partner BioNTech also forecasts a massive increase in sales in 2021 and a net profit of €3.9 billion in the first six months of 2021 (compared with a net loss of € 142 million in the same period last year).[10] BioNTech's stock market value exceeded the US$ 100 billion threshold for the first time in August 2021.[11] The co-founder, CEO and one of the main shareholders of BioNTech Uğur Şahin became a billionaire as a result of the pandemic. According to Forbes magazine, he is one of at least 40 newcomer billionaires who draw their fortunes from companies involved in fighting COVID-19.[12] They are among the main profiteers of the pandemic.
People in the countries of the global South, already facing inequitable vaccine distribution, are also confronted with falling government revenues and rising debt burdens. The situation will worsen as regular vaccine boosters become necessary in the coming years. What is tantamount to a license to print money for the pharmaceutical companies is a massive burden on public budgets. Scientists warned against this background as early as February 2021 in an article in The Lancet:
If governments in resource-constrained settings divert resources from other vaccination programmes or essential health-care services to pay for COVID-19 vaccines and vaccination programmes, health budgets could be distorted with long-term adverse consequences for health and economic development.[13]
Increasing global vaccine production capacity, lowering market prices, and substantially increasing public financial support are vital, especially for the poor and disadvantaged people in the global South.
Technology transfer and patent waiver/release to reduce vaccination inequalities
In May 2020, WHO established the COVID-19 Technology Access Pool (C-TAP) at the initiative of Costa Rica.[14] This aims to pool voluntary licenses, study/research and regulatory data, and existing know-how to accelerate technology transfer to overcome the vaccine shortage. The expectation of C-TAP was to fulfill the goal of making vaccines and other medical technologies truly global public goods. The model was the successful pool for patents and licenses on drugs for AIDS treatment. C-TAP is supported by some 40 countries, including six countries in the global North (Belgium, Luxembourg, the Netherlands, Norway, Portugal and Spain).[15] Most countries with large vaccine production capacity, such as the USA, Germany, China and India, do not support the initiative. Thus, it has so far remained without any noticeable impact.
Faced with scarce global production capacity, India, South Africa, Kenya and Eswatini applied for a waiver under the Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS) in the World Trade Organization (WTO) in October 2020 to temporarily remove patent protection for COVID-19-related vaccines, medicines and devices. The TRIPS waiver is intended to enable manufacturers in the global South in particular to produce medicines and vaccines more quickly and at lower cost (see Special Contribution 1.1 by K.M. Gopakumar of Third World Network). More than 100 countries support this initiative, including the USA as of May 2021.[16] The EU, the UK, Switzerland and the pharmaceutical companies and lobby groups based in these countries are particularly opposed, arguing that the biggest barrier is not the patents, but a lack of production capacity. However, various studies, as the one for example by the NGO Knowledge Ecology International (KEI), show that there are production facilities in numerous countries of the global South, such as Egypt, Brazil, India, Mexico, Morocco, Senegal and South Africa, which could be used or expanded for the production of COVID-19 vaccines.[17]
Winnie Byanyima, Executive Director of UNAIDS, warns:
While the companies making massive profits from COVID vaccines are refusing to share their science and technology with others in order to increase the global vaccine supply, the world continues to face the very real risk of mutations that could render the vaccines we have ineffective and put everyone at risk all over again.[18]
In this context, the more fundamental question arises as to whether medicines vital to realize the human right to health should be patented at all. Should they not in principle be considered global public goods, especially when, as in the case of the COVID-19 vaccines, billions of dollars of public money have gone into research and development? The inventor of the polio vaccine in 1955, Jonas Salk, when asked who owned the patent for his vaccine, responded, “Well, the people, I would say. There is no patent. Could you patent the sun?”[19]
The multi-stakeholder response to COVID-19
In order to accelerate development, production and equitable access to COVID-19 tests, treatments and vaccines, the WHO and several partners—including France, the EU and the Bill & Melinda Gates Foundation --launched the Access to COVID-19 Tools (ACT) Accelerator in April 2020.[20]
This has shifted the centre of the global COVID-19 response from WHO to a multi-stakeholder initiative with its own governance and decision-making structure, thereby further weakening WHO's role in the global health architecture. Further, WHO has handed over the lead for global coordination of COVID-19 immunization to the newly created COVAX initiative (on the risks and side effects of this new example of multi-stakeholderism see Special Contribution 1.2. by Harris Gleckman).[21]
COVAX is the vaccines pillar of the Access to COVID-19 Tools (ACT) Accelerator. It is co-led by the Coalition for Epidemic Preparedness Innovations (CEPI), Gavi and the WHO, alongside key delivery partner UNICEF. COVAX’s initial and very ambitious aim was to guarantee fair and equitable access to COVID-19 vaccines for every country in the world. COVAX should be responsible for the pooled procurement and equitable distribution of COVID-19 vaccines, based on a Fair Allocation Framework developed by WHO.[22]
WHO's Fair Allocation Framework originally envisioned two phases:
1. An initial proportional allocation of doses to countries until all countries reach enough quantities to cover 20% of their population
2. A follow-up phase to expand coverage to other populations. If severe supply constraints persist, a weighted allocation approach would be adopted, taking account of a country’s COVID threat and vulnerability.
With the unilateral approach of the rich countries to vaccine procurement (vaccine nationalism), COVAX has failed in its claim to serve a global coordination function. In view of the fact that the European Commission alone has secured 4.1 billion vaccine doses through bilateral supply contracts, the verbal commitment of its president, Ursula von der Leyen, seems more than hypocritical: “To overcome coronavirus, vaccines must reach all corners of the planet, as soon as possible. COVAX is our best vehicle to ensure universal and equitable access to COVID-19 vaccines.”[23]
COVAX's primary task has been refocused to provide COVID-19 vaccines to the 92 low- and middle-income countries of the global South with the objective to provide at least 2 billion COVID-19 vaccine doses by the end of 2021, including at least 1.8 billion to these 92 countries by early 2022.[24]
Whether this will actually happen is questionable. COVAX announced it has, as of July 2021, contracted 3.8 billion vaccine doses from producers and has purchase options for a further 1.3 billion.[25] However, by 3 September 2021 just 236 million vaccine doses had been delivered via COVAX to 139 countries.[26]
COVAX is funded primarily through voluntary contributions to the COVAX AMC. To date (as of August 2021), it has received pledges of US$ 9.825 billion. In addition, it has received US$ 799 million to support vaccine delivery and/or logistics.
The largest donors are the United States, Germany, Japan, the United Kingdom, the European Commission, and Italy (see Figure 1.3). The largest non-governmental donor is the Bill & Melinda Gates Foundation. Although the Foundation's financial contribution ranks it only 11th among donors, it has a seat on the key bodies of COVAX.[27]
The funds pledged to date are nowhere near enough to provide sufficient vaccines for the around 4 billion people in the 92 poorest countries.
Figure 1.3: COVAX major donors
(in million US$, as of 6 August 2021)
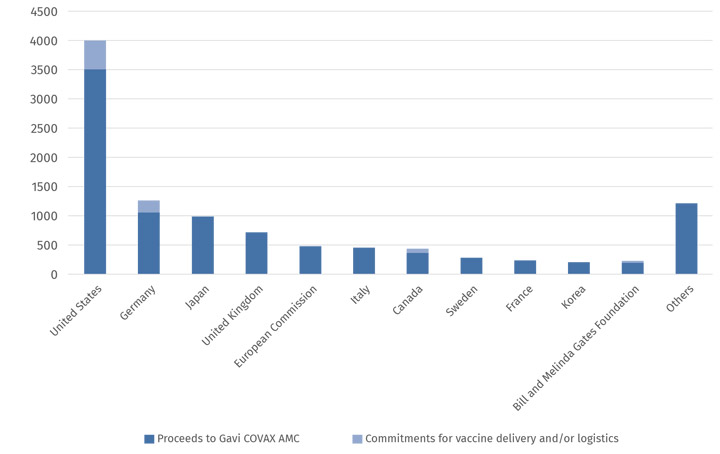
Source: https://www.gavi.org/news/document-library/covax-amc-donors-table
In addition to voluntary financial contributions, COVAX is increasingly receiving ‘in-kind’ donations of surplus vaccine doses from wealthier countries. To date, 16 countries have announced plans to donate 640 million vaccine doses by the end of 2022.[28] The German government plans to donate 100 million vaccine doses by the end of 2021, but only on the premise that all ordered doses will be delivered (which is not expected). COVAX will thus become a ‘thrift shop’ for surplus vaccines from rich countries.
The policy of vaccinating one's own population first and then donating the hoarded surplus doses to the rest of the world is heavily criticized. The WHO Director-General stated:
Not only does this me-first approach leave the world’s poorest and most vulnerable people at risk, it’s also self-defeating. Ultimately, these actions will only prolong the pandemic, the restrictions needed to contain it, and human and economic suffering. Vaccine equity is not just a moral imperative, it is a strategic and economic imperative.[29]
Charity-based or rights-based?
Vaccine equity is a human rights imperative as well as a health one. With the UN Covenant on Economic, Social and Cultural Rights, all signatory States have committed themselves under international law to protect the rights of people who do not live on their territory, within the limits of their financial resources. This extraterritorial state obligation also applies to the right to health. The UN Committee on Economic, Social and Cultural Rights stated this clearly:
Instead of pursuing health isolationism and a race for a vaccine, States should honour their obligations to contribute to the enjoyment of all human rights, including the right to health, globally. The distribution of vaccines and the prioritization of access to them should be organized and supported by international cooperation and assistance, which includes the sharing of benefits of scientific progress and its applications. States parties should therefore develop strategies and mechanisms for a fair distribution of the financial costs associated with research into and the production and distribution of vaccines for COVID-19, including through a reduction in the debt burden for countries that need it. They should also adopt transparent and participatory mechanisms that ensure that prioritization in the global distribution of vaccines is based – as should be the case also at the national level – on medical needs and public health considerations. Such support can be organized by using the WHO-supported COVAX Global Vaccines Facility. [30]
To realize the human right to health as well as the commitments under SDG 3, appeals to goodwill and voluntary initiatives by States are not enough. The COVID-19 pandemic has painfully demonstrated the absence of a global health system. This reality has led the president of the European Council, Charles Michel, and the WHO Director-General, Tedros Adhanom Ghebreyesu, to propose an International Treaty on Pandemic Preparedness and Response. Its goal is to create a legally binding framework and improved global governance structures for pandemic preparedness and response. On 30 March 2021, 26 heads of State and government endorsed this call.[31] Whether it can actually bring progress and help overcome the structural weaknesses of the global health architecture, such as the underfunding of the WHO, is unclear. Depending on its design, it could lead to an actual strengthening of the WHO and its instruments, or to its further weakening by outsourcing pandemic preparedness and response to multi-stakeholder bodies with limited democratic legitimacy (see Special Contribution 1.4 by Nicoletta Dentico of SID).
COVID-19 in a time of inequalities
The unequal race for vaccines is just the tip of the iceberg on growing global inequalities. COVID-19 has revealed and deepened, as if through a burning glass, the structural inequalities within and between countries.
Since the outbreak of the pandemic, the World Bank and the UN have had to repeatedly revise their poverty figures. World Bank experts now estimate the number of people living in extreme poverty, on their measure of less than US$ 1.90 per day, to be 732 million in 2020, 97 million higher than it would have been without COVID-19.[32] For many experts, the World Bank's measure of extreme poverty is inadequate and its threshold too low to provide a realistic picture of poverty in the world. What is agreed, however, is that the number of poor people would have risen much more sharply if governments had not countered with various social protection measures and labour market interventions. According to the World Bank, between 20 March 2020 and 14 May 2021, a total of 3,333 social protection measures have been planned or implemented in 222 countries or territories in response to the economic consequences of the pandemic.[33]
These include one-time or repeated cash transfers, in-kind food/voucher schemes and wage subsidies. Many of these measures were debt-financed and cannot be continued permanently, even in richer countries. In poorer countries, the fiscal space for such measures is less. According to World Bank forecasts, the number of poor people in low-income countries will continue to rise in 2021, while in middle- and high-income countries it will decrease again slightly. The World Bank experts conclude: “Hence, in the poorest countries of the world, the impact of COVID-19 on poverty is not only still present, but it is worsening.”[34]
On the other hand, the global number of billionaires and the extent of their wealth has increased more since the pandemic began than at any time in recent decades. The number of billionaires on Forbes magazine’s annual list of the world’s wealthiest people skyrocketed to an unprecedented 2,755 in March 2021.[35] This were 660 more than a year ago. The net wealth of these billionaires increased to US$ 13.1 trillion, up from US$ 8 trillion in March 2020.
Amazon founder Jeff Bezos, currently the richest man in the world, saw his fortune grow from US$ 113 to US$ 213 billion during the pandemic, reaching a historic high on 8 July 2021.[36] As Amazon cashed in on the stay-at-home deliveries, it also benefitted from the huge rise in stock indices in the course of 2021, as did pharmaceutical and other large corporations. [37]
The massive increase in revenues and profits is the result of deliberate tax and regulatory policies that have favoured transnational corporations and wealthy individuals. The flip side of the coin has been empty public coffers and weakened or privatized public institutions and services. The long-term consequences of this disastrous mix of tax benefits, privatization and crushing debt burdens became evident during the pandemic in many countries (see Special Contribution 1.5 by Daria Cibrario from Public Services International).
Massive relief and stimulus packages
In response to the pandemic, many governments seem to have returned to a more proactive policy for providing public goods and services. They have launched rescue packages and stimulus programmes on a massive scale, particularly compared to other recent crises. The IMF puts the total of additional public spending or foregone revenues and liquidity support between January 2020 and June 2021 at US$ 16.549 trillion globally, or an average of 16 percent of GDP.[38] However, the financial capacity of countries to respond to the consequences of the pandemic and thus their budgetary fiscal support to people and firms has varied widely across countries. While fiscal measures, including guarantees, in response to the COVID-19 pandemic accounted for 46.2 percent of GDP in Italy, 44.8 percent in Japan and 41.4 percent in Germany, some poorer countries in the global South spent less than 1 percent of their GDP, for instance Cameroon (0.9%), Haiti (0.6%), and Malawi (0.5%) (see Figure 1.4).
Figure 1.4: Selected countries with the highest and lowest share of fiscal measures in response to the COVID-19 pandemic
(January 2020 to June 2021, in percent of GDP)
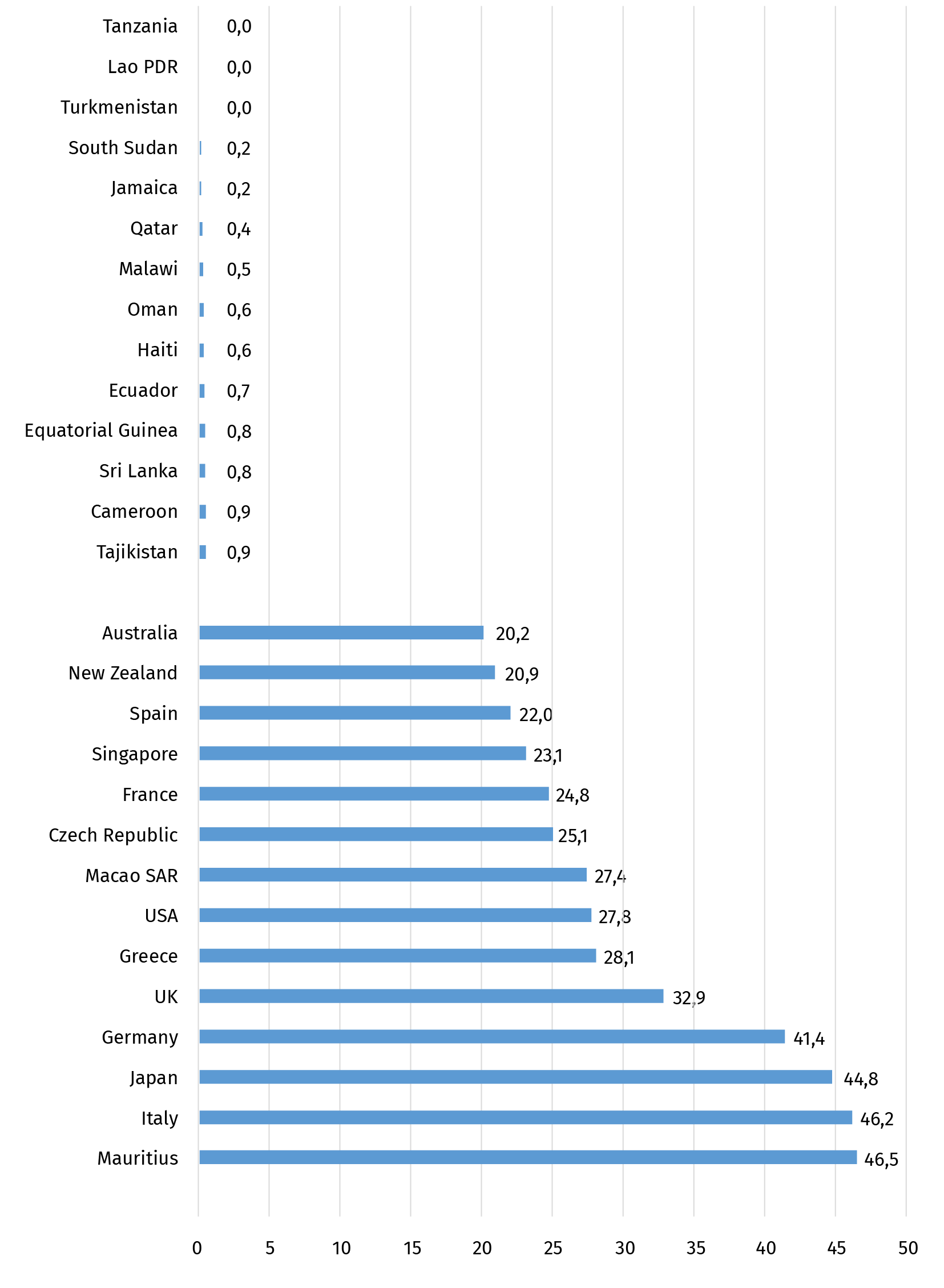
Source: IMF, https://www.imf.org/en/Topics/imf-and-covid19/Fiscal-Policies-Database-in-Response-to-COVID-19
The huge disparities in the fiscal options for responding to the pandemic will further exacerbate socio-economic inequalities between and among countries. There is a risk that the situation will continue to deteriorate in the coming years if countries are forced to switch from expansionary monetary and fiscal policies back to austerity policies with all their negative side effects (see the contribution of Isabel Ortiz and Matthew Cummins in Part 3).
Particularly poorer countries, some of which were already facing massive economic problems before the pandemic, need substantial external support to finance additional healthcare and social spending and measures to overcome the economic recession. But the much-vaunted solidarity of the rich countries has so far not been very forthcoming. In 2020, the official development assistance (ODA) of OECD members rose only incrementally from 0.30 to 0.32 percent of GDP (to a total of US$ 161.2 billion).[39] In some countries, such as the United Kingdom, ODA even decreased due to cuts in their general aid programmes. And the G20's debt-servicing suspension initiative is also woefully inadequate, having provided little more than US$ 5 billion in temporary relief to some 40 eligible countries by the end of 2020.[40] This was less than 2 percent of total debt service due to be paid by developing countries that year. Moreover, the initiative covers only bilateral public debt owed to official creditors but does not apply to the debt owed to private lenders and multilateral creditors. Some of the money saved from debt service suspension is used to pay the private creditors on time and in full – instead of using it for healthcare and other COVID-19 related activities. The initiative is no substitute to urgently needed debt reduction and restructuring for highly indebted countries.[41]
The general allocation of Special Drawing Rights (SDRs) equivalent to US$ 650 billion in August 2021 - the largest distribution ever made by the IMF – has been heralded as a major achievement. However, its distribution will not benefit the countries most in need without rechanneling measures and again illustrates existing imbalances in global economic architecture (see Special Contribution 1.6 by Bodo Ellmers, Global Policy Forum).
Beyond the quantitative increase of fiscal resources to address the COVID-19 crisis, however, the central question is for what purposes the additional resources are being used and who are the main beneficiaries. Over the past year, many UN officials, human rights activists and civil society groups (like in the Spotlight Report 2020) have demanded that the resources of the COVID-19 reconstruction and economic stimulus packages should be used proactively to promote human rights and the implementation of the SDGs.
After one year, initial studies show that this is often not the case. A report of the Financial Transparency Coalition that tracked fiscal and social protection recovery measures in nine countries of the global South found that in eight of them a total of 63 percent of announced COVID-19 funds went to large corporations, rather than small and medium enterprises or social protection measures (see Special Contribution 1.7 by Matti Kohonen of the Financial Transparency Coalition).
Market-based vs. rights -based recovery
But it is not only fiscal measures that are often inconsistent with human rights obligations and the requirements arising from the 2030 Agenda. Certain policy prescriptions and strategies that claim to provide ways out of the global crises are not fully in line with human rights standards and the principles and goals of the 2030 Agenda, and in some cases undermine rather than strengthen democratically legitimized multilateral institutions. This applies not only to the WHO, as mentioned above, but also, for instance, to global institutions in the field of food and nutrition. A striking example is the UN Food Systems Summit in September 2021. Many civil society groups and social movements point out that this Summit is driven by corporate actors like the World Economic Forum (WEF), sidelines existing multilateral bodies such as the Committee on World Food Security (CFS), and focuses mainly on ‘solutions’ that are technology-driven, market-based and capital-intensive[42] (see Special Contribution 1.8 by Magdalena Ackermann, SID, and Charlotte Dreger, FIAN).
UN Secretary-General António Guterres has repeatedly emphasized that human rights must guide all COVID-19 response and recovery measures. This should also mean strengthening the rights of those on the frontlines of the COVID-19 crisis. First and foremost, that means the millions of workers in the healthcare sector. Vanita Mukherjee and Shree Baphna of DAWN point out that around 70 percent of these workers are women, predominantly at the lower ends of the health workers hierarchies. Most of them experience poor work conditions, low wages and job insecurity (see Special Contribution 1.9).
The situation is similar in the education sector. Research by Education International shows that even before the COVID-19 pandemic, teachers’ workloads have steadily worsened, while salaries have remained the same or even decreased. The situation has continued to deteriorate as a result of the pandemic. The global teacher shortage, which the UN estimated at 69 million even before the pandemic, will continue to grow so long as teaching remains to be "an overworked, undervalued, and underpaid profession" (see the Special Contribution 1.10 by David Edwards from Education International).
COVID-19 highlighted the need to re-value the importance of care and education in society, and to fundamentally strengthen public health, social protection and education systems, particularly in light of the climate crisis now urgently upon us. A precondition for this is to reclaim and invest in public goods and services and legislate an economy that protects the human rights of all residents, present and future. States, large and small, must be willing and able to ensure long-term investments and expenditures, not dependent on market solution, with people-centred monetary and fiscal policies – backed up with democratic global economic governance.
[1] UN Doc. A/RES/70/1, para. 14.
[2] https://www.networkideas.org/news-analysis/2021/08/apocalypse-or-cooperation/
[3] https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-148th-session-of-the-executive-board
[4] https://www.who.int/director-general/speeches/detail/director-general-s-opening-remarks-at-paris-peace-forum-spring-meeting-17-may-2021
[5] https://www.unicef.org/supply/covid-19-vaccine-market-dashboard
[6] Own calculation based on https://www.unicef.org/supply/covid-19-vaccine-market-dashboard
[7] Zoltán Kis and Zain Rizvi, How to Make Enough Vaccine for the World in One Year. Washington, D.C.: Public Citizen, 2021, https://www.citizen.org/article/how-to-make-enough-vaccine-for-the-world-in-one-year/
[8] https://annualreview.pfizer.com/files/Pfizer-Annual-Review-2020_Interactive-PDF.pdf and https://investors.pfizer.com/investor-news/press-release-details/2021/PFIZER-REPORTS-SECOND-QUARTER-2021-RESULTS/default.aspx
[9] Ibid.
[10] https://investors.biontech.de/de/investors-media und https://investors.biontech.de/de/news-releases/news-release-details/biontech-veroeffentlicht-ergebnisse-des-zweiten-quartals-2021
[11] https://www.wiwo.de/unternehmen/industrie/boersenwert-biontech-ueberspringt-100-milliarden-dollar-marke/27485444.html
[12] https://www.forbes.com/sites/giacomotognini/2021/04/06/meet-the-40-new-billionaires-who-got-rich-fighting-covid-19/?sh=5c12de4417e5. The People’s Vaccine Alliance listed nine new billionaires with a combined net wealth of US$19.3 billion, enough to fully vaccinate all people in low-income countries 1.3 times, https://www.oxfam.org/en/press-releases/covid-vaccines-create-9-new-billionaires-combined-wealth-greater-cost-vaccinating
[13] https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00306-8/fulltext#fig2
[14] https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/covid-19-technology-access-pool
[15] https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/covid-19-technology-access-pool/endorsements-of-the-solidarity-call-to-action
[16] https://ustr.gov/node/10649
[17] https://www.keionline.org/covid-19-vaccine-manufacturing-capacity
[18] https://www.oxfam.org/en/press-releases/covid-vaccines-create-9-new-billionaires-combined-wealth-greater-cost-vaccinating
[19] Quoted from: https://www.thenation.com/article/society/the-covid-19-vaccine-should-belong-to-the-people/
[20] https://www.who.int/initiatives/act-accelerator
[21] https://www.gavi.org/covax-facility
[22] https://www.who.int/publications/m/item/fair-allocation-mechanism-for-covid-19-vaccines-through-the-covax-facility
[23] https://www.gavi.org/sites/default/files/covid/covax/Gavi-COVAX-AMC-Investment-Opportunity.pdf
[24] https://www.who.int/news/item/27-05-2021-covax-joint-statement-call-to-action-to-equip-covax-to-deliver-2-billion-doses-in-2021
[25] https://www.gavi.org/sites/default/files/covid/covax/COVAX-Supply-Forecast.pdf
[26] https://www.gavi.org/covax-facility
[27] https://www.gavi.org/news/document-library/covax-pillar-structure-and-principles
[28] https://www.gavi.org/news/document-library/covax-dose-donation-table
[29] https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-148th-session-of-the-executive-board
[30] UN Committee on Economic, Social and Cultural Rights (2020): Statement on universal and equitable access to vaccines for the coronavirus disease (COVID-19). Geneva (UN Dok. E/C.12/2020/2) (https://undocs.org/E/C.12/2020/2), para. 11.
[31] Albania, Chile, Costa Rica, the European Council, Fiji, France, Germany, Greece, Indonesia, Italy, Kenya, the Netherlands, Norway, Portugal, the Republic of Korea, Romania, Rwanda, Senegal, Serbia, South Africa, Spain, Thailand, Trinidad and Tobago, Tunisia, the United Kingdom, and Ukraine, https://news.un.org/en/story/2021/03/1088652, see also https://blogs.bmj.com/bmj/2021/05/23/an-international-treaty-for-pandemic-preparedness-and-response-is-an-urgent-necessity/
[32] Daniel Gerszon Mahler et al., Updated estimates of the impact of COVID-19 on global poverty: Turning the corner on the pandemic in 2021? World Bank, https://blogs.worldbank.org/opendata/updated-estimates-impact-covid-19-global-poverty-turning-corner-pandemic-2021.
[33] Ugo Gentilini et al. , Social Protection and Jobs Responses to COVID-19: A Real-Time Review of Country Measures, version 15, World Bank, May 14, 2021, p. 4, https://openknowledge.worldbank.org/handle/10986/33635)
[34] Mahler et al., 2021, op. cit.
[35] https://www.forbes.com/billionaires/
[36] https://www.forbes.com/sites/kenrickcai/2021/08/20/richest-person-in-world-elon-musk-jeff-bezos-bernard-arnault/?sh=51eb664c1f5a
[37] https://www.apple.com/newsroom/pdfs/FY21_Q3_Consolidated_Financial_Statements.pdf (Apple’s FY 2021 ends in September 2021).
[38] https://www.imf.org/en/Topics/imf-and-covid19/Fiscal-Policies-Database-in-Response-to-COVID-19
[39] https://www.oecd.org/dac/financing-sustainable-development/development-finance-data/ODA-2020-detailed-summary.pdf
[40] https://www.worldbank.org/en/topic/debt/brief/covid-19-debt-service-suspension-initiative
[41] https://www.eurodad.org/g20_dssi_shadow_report
[42] See the analysis of Matthew Canfield, Molly Anderson and Philip McMichael, UN Food Systems Summit 2021: Dismantling Democracy and Resetting Corporate Control of Food Systems, Front. Sustain. Food Syst., 13 April 2021, https://doi.org/10.3389/fsufs.2021.661552.